Racial and Ethnic Minorities Receive Less Quality Mental Health Care in the United States
Helen Cooper
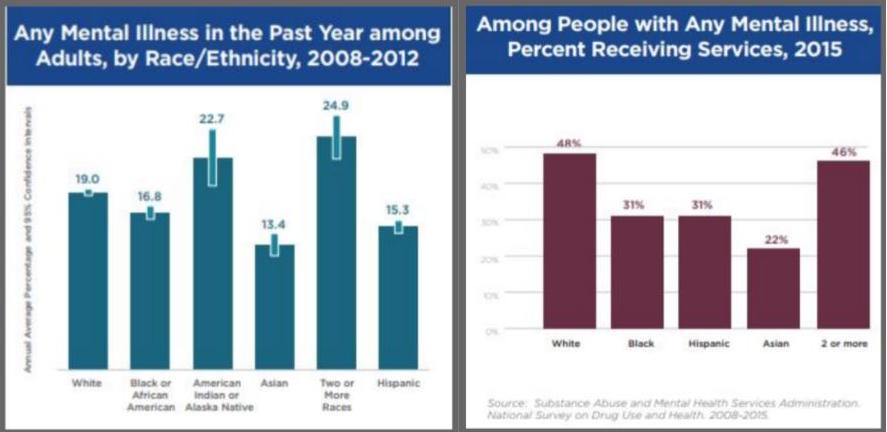
America draws strength from its cultural diversity. Diversity has made our nation a more vibrant and open society, ablaze in ideas, perspectives, and innovations. But the full potential of our diverse, multicultural society cannot be realized until all Americans, including racial and ethnic minorities, gain access to quality health care that meets their needs. According to a report published by the U.S. Department of Health and Human Services, racial and ethnic minorities have less access to mental health services than do Whites. They are also less likely to receive the care they need and if and when they do get it, it is more likely to be poor in quality. (DHHS, 1999) The American Psychiatric Association identified in 2015 that, among adults with any mental illness, 48% of Whites received mental health services, compared to 31% of Blacks and Hispanics, and 22% of Asians. (APA, 2017) Another major conclusion of the Supplement, Mental Health: A report of the Surgeon General, included that racial and ethnic minorities bear a greater burden from unmet mental health needs and thus suffer a greater loss to their overall health and productivity. While studies have not addressed this disability burden for minorities relative to Whites, key findings do show that most minority groups are less likely than Whites to use services, and they receive poorer quality mental health care, despite having similar community rates of mental disorders. (APA, 2011) Similar prevalence, combined with lower utilization and poorer quality of care, means that minority communities have a higher proportion of individuals with unmet mental health needs.
The Supplement provides extensive documentation of the scientific advances illuminating our understanding of mental illness and its treatment. It found a range of effective treatments for most mental disorders. One piece of recommendation that the Surgeon General made applies for all people: Seek help if you have a mental health problem or think you have symptoms of a mental disorder. The advice to seek help is very important; however, the majority of people with diagnosable disorders, regardless of race or ethnicity, do not search for or receive treatment. This is often due to the stigma surrounding mental illness. “People with mental illness feel shame and fear of discrimination about a condition that is as real and disabling as any other serious health condition.” (DHHS, 1999) Additional barriers that deter racial and ethnic minorities are mistrust and fear of treatment, differences in language and communication, and most importantly – racism and discrimination. More broadly, mental health care disparities may also stem from minorities’ historical and present-day racial struggles, which affect their mental health and contribute to their lower economic, social, and political status.
Some studies have begun to track trends in mental health care disparities. Using a national data set (MEPS), Black-White and Hispanic-White disparities in rates of any mental health care use worsened from 2000-2001 to 2003-2004. Using another nationally representative sample of service use (NAMCS), no evidence was found for progress against disparities in depression and anxiety care in either primary care or psychiatric settings over the past decade. Similar findings from a nationally representative sample of English-speaking individuals, overall rates of treatment for psychiatric disorders increased between 1990 and 2003, in both years, but Blacks were only 50% as likely to receive psychiatric treatment as Whites for diseases of similar severity. (DHHS, 1999) In summary, not only do disparities exist in the access and use of mental health services for minority individuals, but efforts to eliminate these imbalances have been unsuccessful in the last decade.
To better understand what happens in the clinical setting, one must look at how culture and society play pivotal roles in mental health and care. The cultures of racial and ethnic minorities influence many aspects of mental illness, including how patients from a given culture communicate and manifest their symptoms, their family and community supports, how much stigma surrounds mental health in their culture, and their willingness to seek treatment. Additionally, some cultures have shown strength in which they have the ability to be “resilient” and use adaptive ways of coping. This has led to some cultures being able, to an extent, to prevent the development of certain disorders in their community.
However, don’t be fooled! Culture is in no way limited to just the patients themselves – it involves the professionals who treat them, too. Every group of professionals embodies a “culture” in the sense that they too have a shared set of beliefs, norms, and values. Due to advancements in Western medicine, which strives to uncover universal truths about disease, most clinicians share a worldview about the interrelationship between body, mind, and environment informed by knowledge acquired through the scientific method. It also means that clinicians view symptoms, diagnoses, and treatments in ways that sometimes diverge from their clients’ views, especially when the cultural backgrounds of the consumer and provider are dissimilar. This divergence of viewpoints can create barriers to effective care. Clinicians offer a huge influence on the delivery of care, including diagnosis and treatment. Unfortunately, provider discrimination, including bias and stereotyping, is another source of disparities; however, there has not been any further research done to show a link between the two. (Institute of Medicine of the National Academie, 2002)
So what are some ways in which we can increase equal opportunity to quality mental health care and reduce disparities for racial and ethnic minorities? There is no straightforward answer and solutions to the issue can be controversial. Reducing or eliminating these disparities requires a steadfast commitment by all sectors of American society. Luckily, the U.S. Department of Health and Human Services has a vision for the future. The published Supplement suggests multiple pieces of recommendation, including the continuing expansion of the science base. Science is key to building a good public health approach to mental health and illness. The science base regarding racial and ethnic minority mental health is limited but growing. Since 1994, the National Institutes of Health (NIH) has required inclusion of ethnic minorities in all NIH-funded research. (NIH Guidelines, 1994, p. 14509) When combined with smaller, ethnic-specific epidemiological ones, these surveys may help resolve some of the uncertainties about the extent of mental illness among racial and ethnic groups. Additionally, they will also make the understanding of how factors such as acculturation, stigma, ethnic identity, racism, and spirituality provide protection from or risk for, mental illness in racial and ethnic minority populations. “With these groundbreaking studies, the mental health field will gain crucial insight into how social and cultural factors operate across race and ethnicity to affect mental illness in diverse communities.” (DHHS, 1999) Another major source of improvement comes from improving the access and quality of mental health services. Due to many racial and ethnic minorities living in areas where access to care is not readily available, one major course of action is to improve geographic availability of mental health services. Another major step in improving mental health services is to improve language access. Strengthening the communication between clinicians and patients is essential to mental health care. Finally, to improve quality of care and be most effective, treatments always need to be individualized in the clinical setting according to each patient’s age, gender, race, ethnicity, and culture (DHHS, 1999).
Reducing barriers is another place for refinement. Mental Health: A Report of the Surgeon General (DHHS, 1999) highlights the importance of facilitating entry into treatment, reducing financial barriers, and overcoming the stigma regarding mental illnesses. The Supplement strives to ensure parity and expansion of public health insurance, as well as extend health insurance for the uninsured. Yet another problem of disparity arises when supporting capacity development. “Minorities are underrepresented among mental health providers, researchers, administrators, policymakers, and consumer and family organizations. Furthermore, many providers and researchers of all backgrounds are not fully aware of the impact of culture on mental health, mental illness, and mental health services.” (DHHS, 1999) To help solve this issue, the Supplement encourages all mental health professionals to develop their skills in tailoring treatment to age, gender, race, ethnicity, and culture. Additionally, maximization of care can be done by promoting leadership within communities where mental health systems are located. Patients and their families will be able to address any problems they have and be engaged in the planning and implementation of their mental health services. To reduce disparities in knowledge, and the availability, utilization, and quality of mental health services for racial and ethnic minority consumers, mental health programs must develop a climate that conveys an appreciation of diverse cultures and an understanding of the impact of these cultures on mental health and mental illness. By doing this, providers can ensure that all the needs of the patient and their families are met, including racial and ethnic minorities.
Last but certainly not least, mental health must be more widely promoted! Encouraging the open discussion of mental illness can improve the overall health of a community and the nation. Many factors such as poverty, community violence, racism, and discrimination can adversely affect mental health, and therefore the reduction in these conditions is crucial to improvement of mental health for racial and ethnic minorities. Instead, care should be focused on using natural community or cultural strengths such as spirituality, positive ethnic identity, traditional values, educational attainment, and local leadership to prevent mental illness. Strengthening bonds between patients and their families is also essential in the healing process. “Families are the primary source of care and support for the majority of adults and children with mental problems or disorders. Efforts to promote mental health for racial and ethnic minorities must include strategies to strengthen families to function at their fullest potential and to mitigate the stressful effects of caring for a relative with a mental illness or a serious emotional disturbance.” (DHHS, 1999)
It is no secret that there is compelling evidence that shows that racial and ethnic minorities collectively experience a disproportionately high disability burden from unmet mental health needs compares to Whites. While much progress has been made in understanding mental illness and advancing in treatment, there is still so much to learn about different racial and ethnic groups within the United States. As quoted by the Surgeon General of the Supplement, “The Nation has far to go to eliminate racial and ethnic disparities in mental health. While working toward this goal, the public health system must support the strength and resilience of America’s families. The demographic changes anticipated over the next decades magnify the importance of eliminating differences in mental health burden and access to services. Ethnic minority groups are expected to grow as a proportion of the total U.S. population. Therefore, the future mental health of America as a whole will be enhanced substantially by improving the health of racial and ethnic minorities.” (DHHS, 1999) Addressing disparities in mental health is the right thing for all Americans to do. Without a healthy mind, it is hard for your body to function properly, too. Mental health is just as serious and important and physical health and should not be restricted to certain races or ethnicities anywhere around the globe. Ensuring that everyone has equal and quality mental health care in the United States is the next big step in becoming a more unified nation.